Sitting here on the eve of Riley’s 5th birthday, I remember how much pain I was in five years ago; I was on the edge of almost 30 hours of (active) labor. At the time I couldn’t even fathom five years down the road, having a preschool grad and talking about kindergarten. But I did think by that time I would have already gone through pregnancy again and we’d have an almost 5year old and a baby or toddler. Someday still maybe, but at least for the current present, Riley is all that matters. The fact that we’re going to be celebrating his 5th birthday is so huge. I can vividly remember when we were unsure if he’d make it to his 3rd birthday and highly questioned his 4th. Despite everything he and we have been through in the last five years with his health, I’m genuinely surprised and over the moon with how stubborn, strong and stable he is right now. It gives me hope for the next five years. I know how precious life is with him and how that can quickly change, but for once…I have more hope than I thought possible.
Without hope of Riley’s continued goofy smiles, things can get rough. I admit, that I’ve battled depression for probably the past four years or so. When things are good, it makes it that much easier to make me feel the same way. And when things are bad, I’m usually numb and so focused on him for a good period of time, until it sinks in and then it’s a slow climb back to some sort of normalcy. But I’ve “learned” how to manage it, by taking care of myself when I can, focusing on a lot of positives, returning to work and doing something I actually like, etc.
I thrive on routines and lists though, and the past several months it’s been shaken up so much with changes. As boring as it can be to go stretches of a specific daily routine, I miss it. I started working for Encompass as a Family Resource Coordinator in Birth to Three Early Intervention in November and am now working with the group of people who supported Riley and us through his therapies when he was younger, and I’m loving getting to do something that I care about. Not to mention the flexibility that I am grateful for, to also handle Riley’s care. But then Riley got a GI deal that sent us to the hospital for almost 2 months and I had to figure out how to juggle that and work. Although on the boring days waiting around the hospital, I was so thankful for something other than Netflix to distract me.
And now we’ve been home for a little over a month. Riley went back to school for three weeks, so adjusted to that routine again, and now he’s done with preschool (say WHAT?) and off for summer break. Shortly after he finished, my dad officially retired. Which still hasn’t sunk in yet, even though he’s watched Riley a handful of times already by himself without my mom around. And here in the next few days, my mom will be on summer break too. I’m thankful to have both of them free to watch Riley when needed, especially since I don’t have the summer off work (minus a week of family vaca in CA and a long weekend in Napa). But once again, it’s a new routine to get used to, that won’t exactly be the same from week to week. So, I make my lists and just figure out each week at a time, learn how to “go with the flow”, which I’m not always a fan of, but if I’ve learned how to live day by day with Riley’s health and care, I trust that I can adapt myself to some flexibility.
Doing the math, he’s spent roughly 15% of his life in the hospital for one reason or another. And that’s just what I can remember and count up. If you take into account what I’m missing and many random ER trips (which I don’t even bother trying to remember dates), I’m sure it’s closer to 20%. A fifth of his life, and it’s his 5th birthday…a whole (insert so many swear words here) YEAR. It almost doesn’t seem possible because we’ve only had two really long trips, but we’ve had many several week-ers, many handful of days, and the longest stretch we’ve gone without a trip for whatever reason…roughly 8 months. From June 2016 to March 2017, and that was after we were on edge after almost losing him, he got to meet all his extended crazy Corkery family, and we got his Make-A-Wish trip in to Mickey’s house in Florida in because we were afraid of putting it off.
There are so many days when I don’t think I can take it. Times I wonder what life would be like if I hadn’t found out I was pregnant. The weight on a parent’s shoulders of the high care a medically fragile special needs child requires, the worry if you’re doing enough and doing it right, the stares from strangers, the different ways you have to do so many things to accommodate your kid, is… for lack of a better word, a lot. But in the end, I would give my life for this boy. I would go to the ends of the earth for him, because I can’t even fathom my life without him. A reality where I hadn’t found out I was pregnant with him, is just static. He is our world, he is worth it, he is the best gift ever. And that outweighs everything.
We have good friends getting married this weekend, and we’re so excited to celebrate them and with them. Also makes me realize that Chris and I have been together now for over 11 years and married 7 in July. We spent our 20’s together in college, buying our first cars, falling in love, having fun with friends, getting married, buying a home, getting a dog, getting a very big surprise on a “pee-stick”, having a beautiful baby boy, finding out that he has some sort of underlying neurodegenerative disease, and almost loosing him. Man, that’s a lot of shit. Good and bad. Happy and sad. I’ll be 32 at the end of next month, and Chris 33 in December. Our thirties have started out more adult. We have this amazing goofy happy KID (not baby…. not toddler…not little boy…. KID, 5-YEAR-OLD KID), who loves us both fiercely, adores his grandparents and uncles, and has such joy being around friends (his uncles and aunties, and his own age buddies). Despite how shit hits him when he’s sick, he’s a fighter and finds a way to bounce back and tell docs they’re wrong. We’re finishing a refi on our home that will allow us to do a lot of adult work to it, like exterior painting, expanding the front porch and back decks, new fencing, landscaping, and most importantly, installing an exterior lift for our growing KID. I have to admit, I’m fairly pleased with how our thirties are starting.
I’m still a bit in shock at him turning five, and the fact that I can tell that he’s understanding the meaning of it, and so excited for his birthday. I’ve been doing a count down each day this week about how many days left and how old he’s turning with his fingers on his hand, and how he’s going to be a whole hand-years old. Smiles, giggles, coos of excitement. Thinking of our developmental evaluations at work, and areas of development, I’ve seen so much improvement since he’s started school in his receptive language. You can tell, especially with certain things and repeating things several times (like each day we talk about his bday), that he’s getting it. And probably way more than I’m even giving him credit for. And his social emotional interactions have gone through the roof as well. We were so nervous about preschool, one of the scariest decisions letting strangers basically handle his care, but it was one of the best decisions we’ve ever made. He’s grown so much and grown into this awesome kid. I could not be prouder of him, in every way possible.
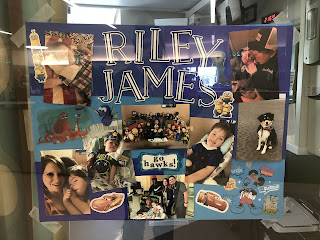
Happy (almost) 5th birthday Riley Bear, Mommy and Daddy love you more than we can even say. We are so proud of the kid you’ve become, the strength you have, the adorable goofiness you possess, the smiles that light up an entire room. You may not be able to sit on your own, or run around the house, but that is what we are here for, to be that strength, comfort and entertainment, so you don’t even know what you’re missing. Because you are perfect just the way you are. We love you Riley James, happy birthday (tomorrow) baby.